Mohs Skin Cancer Surgery

The following information has been taken from the pamphlet, “Important Patient Information Regarding Mohs Micrographic Surgery in the Treatment of Skin Cancer”, provided by the American Society for Mohs Surgery.
What is Mohs Micrographic Surgery?
Mohs micrographic surgery is a specialized, highly effective technique for the removal of skin cancer. The procedure was developed in the 1930s by Dr. Frederic Mohs at the University of Wisconsin and is now practiced throughout the world. Mohs surgery differs from other skin cancer treatments in that it permits the immediate and complete microscopic examination of the removed cancerous tissue, so that all “roots” and extensions of the cancer can be eliminated. Due to the methodical manner in which tissue is removed and examined, Mohs surgery has been recognized as the skin cancer treatment with the highest reported cure rate.
The Mohs Surgical Procedure
Typically, Mohs surgery is performed as an outpatient procedure in the physician’s office. Although the patient is awake during the entire procedure, discomfort is usually minimal and no greater than it would be for more routine skin cancer surgeries. The Mohs surgical procedure is illustrated in the following diagrams:
Stage 1
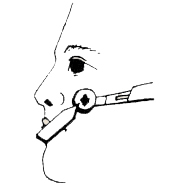
Figure A
The area to be treated is cleansed, marked, and injected with a local anesthetic. The Mohs surgeon removes the visible cancer, along with a thin layer of additional tissue (Stage 1). This procedure takes only a few minutes, and the patient waits while tissue is being processed and examined.
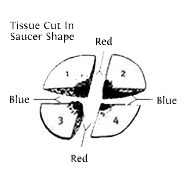
Figure B
The removed tissue specimen is cut into sections, stained, and marked on a detailed diagram (Mohs map).
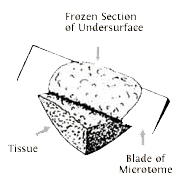
Figure C
Tissue is frozen on a cryostat, and technician removes very thin slices from the entire edge and undersurface. These slices are then placed on slides and stained for examination under the microscope. (This is the most time-consuming portion of the procedure, often requiring one hour or more to complete.)
Stage 2
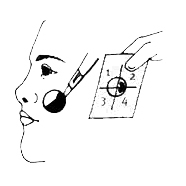
Figure D
The Mohs surgeon carefully examines the entire undersurface and complete edge of the specimen, and all microscopic “roots” of the cancer are precisely identified and pinpointed on the Mohs map. Upon microscopic examination, if residual cancer is found, the Mohs surgeon utilizes the Mohs map to direct the removal of additional tissue (Stage II). Note that additional tissue is removed only where cancer is present.
Stage 3
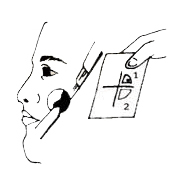
Figure E
This process is repeated as many times as necessary to locate any remaining cancerous areas within the tissue specimen (Stage III, Stage IV, etc.)
Stage 4
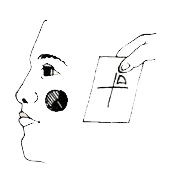
Figure F
When microscopic examination reveals that there is no remaining tumor, the surgical defect is ready for repair.
More about Mohs
Click on a topic to learn more.
